หน้าหลัก | สุขภาพดี | สุภาพสตรี | การแปลผลเลือด | โรคต่างๆ | วัคซีน | อาหารเพื่อสุขภาพ
กินไขมันอย่างไรจึงจะป้องกันโรค
ไขมันในอาหาร มีความสำคัญต่อกระบวนการต่างๆ ของร่างกาย เช่น ช่วยเคลื่อนย้ายวิตามินไปทั่วร่างกายและช่วยสร้างฮอร์โมน
ไขมันในอาหารมี 4 ชนิด ได้แก่ ไขมันอิ่มตัว ไขมันไม่อิ่มตัวเชิงเดี่ยว ไขมันไม่อิ่มตัวเชิงซ้อน และไขมันทรานส์ ไขมันแต่ละชนิดมีผลต่อคอเลสเตอรอลในเลือด ด้วยเหตุนี้ จึงแนะนำให้เปลี่ยนอาหารและเครื่องดื่มที่มีไขมันอิ่มตัว และไขมันทรานส์สูงด้วยอาหารอื่นที่มีไขมันไม่อิ่มตัวเชิงซ้อนหรือไม่อิ่มตัวเชิงเดี่ยวมากกว่า
ไขมันในอาหารมีจำนวนพลังงานเท่ากับ 9 แคลอรีต่อกรัม มากกว่าคาร์โบไฮเดรตหรือโปรตีน (4 แคลอรีต่อกรัม) มากกว่าสองเท่า ทำให้มี 'พลังงานหนาแน่น' มาก
อาหารที่มีไขมันสูงมักจะมีแนวโน้มที่จะเพิ่มไขมันในร่างกาย ดังนั้น ขอแนะนำให้เลือกตัวเลือกอาหาร 'ไขมันต่ำ' หากคุณมีปัจจัยเสี่ยงต่อการเกิดโรคหัวใจ โรคเบาหวาน
ประเภทของไขมันในอาหาร
ไขมันในอาหารแบ่งออกได้เป็น 4 ประเภท เหล่านี้คือ:

ไขมันแต่ละชนิดจะทำงานภายในร่างกายแตกต่างกันและมีผลต่อระดับไขมันในเลือดต่างกัน
1.ไขมันอิ่มตัว
ไขมันอิ่มตัว (บางครั้งเรียกว่า 'ไขมันเลว') มีส่วนทำให้เกิดความเสี่ยงต่อโรคหัวใจและหลอดเลือด (เช่น โรคหัวใจและหลอดเลือด) เนื่องจากไขมันเหล่านี้ทำให้ระดับคอเลสเตอรอล LDL ในเลือดสูงขึ้น
ไขมันเหล่านี้มักพบในอาหารและเครื่องดื่ม เช่น อาหารซื้อกลับบ้านที่ใช้พลังงานสูง ('ฟาสต์ฟู้ด') และผลิตภัณฑ์เชิงพาณิชย์บางอย่าง (เช่น บิสกิตและขนมอบ)
ไขมันอิ่มตัวยังพบได้ในอาหารเพื่อสุขภาพบางชนิดในชีวิตประจำวัน (เช่น ผลิตภัณฑ์จากนมและเนื้อสัตว์)
ไขมันอิ่มตัวพบได้ในอาหารหลายชนิดทั้งคาวและหวาน ส่วนใหญ่มาจากสัตว์ ได้แก่ เนื้อสัตว์และผลิตภัณฑ์จากนม ตลอดจนอาหารจากพืชบางชนิด เช่น น้ำมันปาล์ม อาหารที่มีไขมันอิ่มตัวสูง ได้แก่
ไขมันอิ่มตัวเสี่ยงต่อสุขภาพ
ร่างกายของเราสร้างคอเลสเตอรอลจากไขมันที่เรารับประทานเข้าไป
โคเลสเตอรอลส่วนใหญ่สร้างในตับจากไขมันที่คุณรับประทานเข้าไป มันถูกพาเข้าสู่กระแสเลือดได้สองทาง:
การรับประทานไขมันและน้ำตาลมากเกินไปสามารถเพิ่มระดับของไตรกลีเซอไรด์ ซึ่งเป็นสารไขมันที่ส่วนใหญ่สร้างจากตับ ระดับไตรกลีเซอไรด์ในเลือดสูงยังเชื่อมโยงกับการตีบตันของหลอดเลือดแดงอีกด้วย
ปริมาณไขมันอิ่มตัวที่เรารับประทาน
ผู้ชายโดยเฉลี่ยควรตั้งเป้าที่จะรับประทานไขมันอิ่มตัวไม่เกิน 30 กรัมต่อวัน
ผู้หญิงโดยเฉลี่ยควรจะรับประทานไขมันอิ่มตัวไม่เกิน 20 กรัมต่อวัน
เด็กควรมีน้อยลง
การลดไขมันอิ่มตัว
ใช้คำแนะนำที่เป็นประโยชน์เหล่านี้เกี่ยวกับอาหารทั่วไปเพื่อช่วยลดไขมันอิ่มตัว
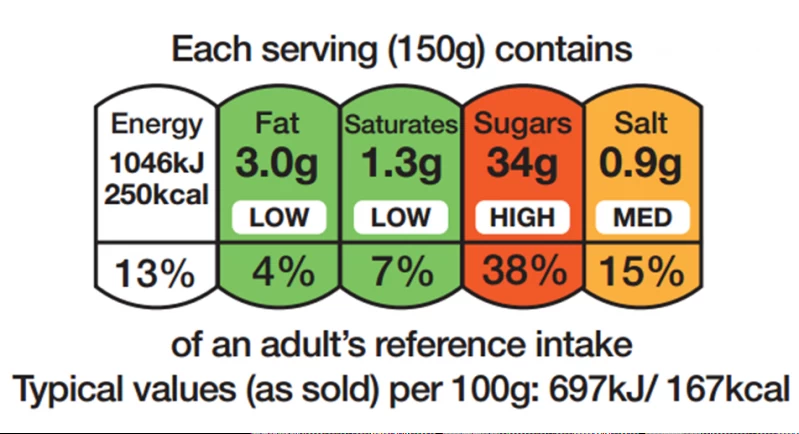
อ่านฉลาก
ฉลากโภชนาการสามารถช่วยคุณลดไขมันอิ่มตัวได้ มองหา "saturates" หรือ "sat fat" บนฉลาก
ฉลากด้านล่างเป็นตัวอย่างที่จัดทำโดยซูเปอร์มาร์เก็ตชั้นนำ ซึ่งแสดงให้เห็นอย่างชัดเจนว่าอาหารมีไขมันอิ่มตัวสูง เนื่องจากส่วนอิ่มตัวเป็นรหัสสีแดง
2.ไขมันไม่อิ่มตัว
หากคุณต้องการลดความเสี่ยงของโรคหัวใจ ควรลดปริมาณไขมันโดยรวมและเปลี่ยนไขมันอิ่มตัวเป็นไขมันไม่อิ่มตัว มีหลักฐานที่ดีว่าการแทนที่ไขมันอิ่มตัวด้วยไขมันไม่อิ่มตัวสามารถช่วยลดคอเลสเตอรอลได้
ไขมันไม่อิ่มตัวพบมากในน้ำมันจากพืช ไขมันไม่อิ่มตัวสามารถเป็นได้ทั้ง
ไขมันไม่อิ่มตัวเชิงเดี่ยวพบได้ใน:
ไขมันไม่อิ่มตัวเชิงซ้อนสามารถช่วยลดระดับของคอเลสเตอรอลชนิดเลวได้ การเปลี่ยนไขมันอิ่มตัวด้วยไขมันไม่อิ่มตัวเชิงซ้อนอาจช่วยลดระดับไตรกลีเซอไรด์ได้เช่นกัน
ไขมันไม่อิ่มตัวเชิงซ้อนมี 2 ประเภท ได้แก่
ไขมันโอเมก้า 3 และโอเมก้า 6 บางประเภทร่างกายสร้างเองไม่ได้ ดังนั้นจึงจำเป็นต้องได้รับในปริมาณเล็กน้อยในอาหาร
ไขมันโอเมก้า 6 พบได้ในน้ำมันพืช เช่น เรพซีด ข้าวโพด ทานตะวัน และถั่วบางชนิด ไขมันโอเมก้า 3 พบได้ในปลาที่มีน้ำมัน เช่น ปลาแมคเคอเรล ปลาคิปเปอร์ ปลาเฮอริ่ง ปลาเทราต์ ปลาซาร์ดีน ปลาแซลมอน และปลาทูน่าสด
ในขณะที่พวกเราส่วนใหญ่ได้รับโอเมก้า 6 อย่างเพียงพอในอาหารของเรา ส่วนใหญ่มาจากน้ำมันปรุงอาหาร เราแนะนำให้กินโอเมก้า 3 ให้มากขึ้นโดยกินปลาอย่างน้อย 2 ส่วนต่อสัปดาห์ รวมถึงปลาที่มีน้ำมันด้วย
แหล่งผักที่มีไขมันโอเมก้า 3 ไม่ได้คิดว่ามีประโยชน์ต่อสุขภาพหัวใจเช่นเดียวกับที่พบในปลา
ประโยชน์ของกรดไขมันโอเมก้า 3
การวิจัยกำลังดำเนินอยู่ แต่ประโยชน์ของกรดไขมันโอเมก้า 3 ในอาหารดูเหมือนว่า:
แหล่งที่มาของกรดไขมันโอเมก้า 3 จากพืชอย่างไรก็ตามร่างกายไม่ได้แปลงและนำไปใช้เช่นเดียวกับโอเมก้า 3 จากปลา
อาหารที่ประกอบด้วยไขมันไม่อิ่มตัวเชิงเดี่ยวและไขมันไม่อิ่มตัวเชิงซ้อนส่วนใหญ่จะเป็นของเหลวที่อุณหภูมิห้อง เช่น น้ำมันมะกอก น้ำมันดอกคำฝอย น้ำมันถั่วลิสง และน้ำมันข้าวโพด ปลาที่มีกรดไขมันโอเมก้า 3 สูง ได้แก่ ปลาแซลมอน ปลาทูน่า ปลาเทราต์ ปลาแมคเคอเรล ปลาซาร์ดีน และปลาเฮอริ่ง แหล่งที่มาของกรดไขมันโอเมก้า 3 จากพืช ได้แก่ เมล็ดแฟลกซ์ (บด) น้ำมัน (คาโนลา เมล็ดแฟลกซ์ ถั่วเหลือง) ถั่วและเมล็ดพืชอื่นๆ (วอลนัท บัตเตอร์นัท และทานตะวัน)
2.1ไขมันไม่อิ่มตัวเชิงเดี่ยว
ไขมันไม่อิ่มตัวเชิงเดี่ยวและไม่อิ่มตัวเชิงซ้อน (บางครั้งเรียกว่า 'ไขมันดี') มีแนวโน้มที่จะ ลดคอเลสเตอรอล LDL ในเลือดของคุณ เมื่อแทนที่ไขมันอิ่มตัวในอาหาร
แหล่งอาหารไขมันไม่อิ่มตัวเชิงเดี่ยว ได้แก่
2.2ไขมันไม่อิ่มตัวเชิงซ้อน
ไขมันไม่อิ่มตัวเชิงซ้อนมีความสามารถในการลดคอเลสเตอรอล LDL มากกว่าไขมันไม่อิ่มตัวเชิงเดี่ยวเล็กน้อย ไขมันไม่อิ่มตัวเชิงซ้อนมี 2 ประเภท ได้แก่
แหล่งอาหารไขมันไม่อิ่มตัวเชิงซ้อน ได้แก่
หากเป็นไปได้ ให้เปลี่ยนอาหารและเครื่องดื่มที่มีไขมันอิ่มตัวสูงด้วยอาหารที่ไม่อิ่มตัวเชิงเดี่ยวหรือไม่อิ่มตัวเชิงซ้อน ตัวอย่างเช่น
3ไขมันทรานส์
ไขมันทรานส์พบได้ตามธรรมชาติในระดับต่ำในอาหารบางชนิด เช่น ไขมันจากสัตว์ รวมถึงเนื้อสัตว์และผลิตภัณฑ์จากนม ไขมันทรานส์ยังสามารถพบได้ในอาหารแปรรูปบางชนิด (เช่น พาย ขนมอบ เค้ก ขนมปังกรอบและขนมปัง) และในอาหารทอดกรอบ
ไขมันทรานส์สามารถพบได้ในน้ำมันพืชที่เติมไฮโดรเจน น้ำมันพืชเติมไฮโดรเจนต้องระบุในรายการส่วนผสมของอาหาร หากมี
เช่นเดียวกับไขมันอิ่มตัว ไขมันทรานส์สามารถเพิ่มระดับคอเลสเตอรอลในเลือดได้ ด้วยเหตุนี้จึงมีคำแนะนำว่าไขมันทรานส์ไม่ควรเกิน 1% ของพลังงาน ที่เราได้รับจากอาหารของเรา สำหรับผู้ใหญ่ ไม่เกิน2.2 กรัมต่อวัน
ไขมันทรานส์มีแนวโน้มที่จะทำตัวเหมือนไขมันอิ่มตัวในร่างกายทำให้
ทำให้เพิ่มความเสี่ยงต่อโรคหัวใจและหลอดเลือด (เช่น โรคหัวใจและหลอดเลือด)
ไขมันเลวและไขมันดี
ไขมันในปริมาณเล็กน้อยเป็นส่วนสำคัญของการรับประทานอาหารที่ดีต่อสุขภาพและสมดุล
ไขมันที่คุณกินเข้าไปจะถูกย่อยสลายระหว่างการย่อยเป็นไขมันหน่วยเล็กๆ ที่เรียกว่ากรดไขมัน ไขมันที่เซลล์ร่างกายของคุณไม่ได้ใช้หรือสร้างพลังงานจะถูกเปลี่ยนเป็นไขมันในร่างกาย ในทำนองเดียวกัน คาร์โบไฮเดรตและโปรตีนที่ไม่ได้ใช้จะถูกเปลี่ยนเป็นไขมันในร่างกายด้วย
ไขมันทุกชนิดให้พลังงานสูง ไขมัน 1 กรัม ไม่ว่าจะอิ่มตัวหรือไม่อิ่มตัว ให้พลังงาน 9kcal เมื่อเทียบกับคาร์โบไฮเดรตและโปรตีนจะให้พลังงาน4kcal สำหรับไขมันประเภทหลักที่พบในอาหาร ได้แก่ ไขมันอิ่มตัวและไขมันไม่อิ่มตัว ไขมันและน้ำมันส่วนใหญ่มีทั้งไขมันอิ่มตัวและไม่อิ่มตัวในสัดส่วนที่ต่างกัน
ส่วนหนึ่งของอาหารเพื่อสุขภาพ เราควรพยายามลดอาหารและเครื่องดื่มที่มีไขมันอิ่มตัวและไขมันทรานส์ และแทนที่ด้วยไขมันไม่อิ่มตัว การกินพลังงานมากเกินความจำเป็นบ่อยๆ ไม่ว่าจะเป็นไขมัน คาร์โบไฮเดรต หรือโปรตีน จะเพิ่มความเสี่ยงในการมีน้ำหนักเกินหรือเป็นโรคอ้วน ซึ่งสามารถเพิ่มคอเลสเตอรอลได้ ไขมันแบ่งออกเป้น
1.ไขมันเลวหรือไขมันที่เป็นอันตราย
ที่อาจเป็นอันตรายมีอยู่ 2 ประเภทหลัก ได้แก่
2.ไขมันที่ดีต่อสุขภาพ
ประเภทของไขมันในอาหารที่อาจเป็นประโยชน์ส่วนใหญ่เป็นไขมันไม่อิ่มตัว:
สเตอรอลจากพืชสามารถลดโคเลสเตอรอลได้
สเตอรอลจากพืชเป็นส่วนประกอบในพืชทุกชนิดที่มีโครงสร้างคล้ายกันมากกับโคเลสเตอรอลของมนุษย์ การบริโภคสเตอรอลจากพืช 2 ถึง 3 กรัมต่อวันสามารถลดระดับคอเลสเตอรอลในเลือดได้โดยเฉลี่ย 10% เนื่องจากมันไปปิดกั้นความสามารถของร่างกายในการดูดซึมคอเลสเตอรอล ซึ่งนำไปสู่การลดระดับของคอเลสเตอรอลในเลือด
อย่างไรก็ตาม เป็นเรื่องยากที่จะรับประทานสเตอรอลจากพืชในปริมาณนี้จากแหล่งธรรมชาติ ดังนั้นปัจจุบันจึงมีเนยเทียมและผลิตภัณฑ์จากนมที่อุดมด้วยสเตอรอลจากพืชในท้องตลาด
การรับประทานมาการีนเสริมสเตอรอล 1 ถึง 1.5 ช้อนโต๊ะ (4 ถึง 6 ช้อนชา) ในแต่ละวันสามารถช่วยลดระดับคอเลสเตอรอลในเลือดได้
กรดไขมันจำเป็นในอาหารของเรา
กรดไขมันจำเป็นคือกรดไขมันที่ร่างกายไม่สามารถสร้างขึ้นจำเป็นต้องได้รับจากอาหาร ได้แก่กรดไขมันไม่อิ่มตัวเชิงซ้อนที่จำเป็น 2 ชนิด คืิอ โอเมก้า 3 และโอเมก้า 6 ดังนั้นเราต้องบริโภคกรดไขมันเหล่านี้ในอาหารของเรา
กรดไขมันโอเมก้า 3 พบได้ทั้งในพืชและอาหารจากทะเล แม้ว่าจะเป็นกรดไขมันโอเมก้า 3 จากแหล่งทะเลที่มีหลักฐานชัดเจนที่สุดว่ามีประโยชน์ต่อสุขภาพ (รวมถึงการลดความเสี่ยงของโรคหัวใจ)
แหล่งอาหารจากพืช ได้แก่ คาโนลาและน้ำมันถั่วเหลือง เนยเทียมและเมล็ดพืชที่มีคาโนลาเป็นส่วนประกอบ
แหล่งที่มาทางทะเล ได้แก่ ปลา โดยเฉพาะปลาที่มีน้ำมันมาก (เช่น ปลาแซลมอนแอตแลนติก ปลาแมคเคอเรล ปลาทูน่าครีบน้ำเงินตอนใต้ ปลาสำลี และปลาซาร์ดีน)
กรดไขมันโอเมก้า 6 ส่วนใหญ่พบในถั่ว เมล็ดพืช และน้ำมันจากพืช (เช่น มะกอก ข้าวโพด ถั่วเหลือง และดอกคำฝอย)
คำแนะนำในปัจจุบันเกี่ยวกับไขมันในอาหารของคุณ
แนวทางการบริโภคอาหารของออสเตรเลีย แนะนำ:
เราแนะนำให้กินไขมันให้น้อยลง โดยเฉพาะไขมันอิ่มตัว
คุณสามารถใช้ตัวเลขเหล่านี้เพื่อเป็นแนวทางในการเลือกซื้อของ เมื่อคุณดูฉลากโภชนาการ
เคล็ดลับในการกินไขมันให้น้อยลง
เคล็ดลับเหล่านี้สามารถช่วยคุณลดปริมาณไขมันทั้งหมดในอาหารของคุณ:
การซื้ออาหารที่มีไขมันต่ำ
มีแนวทางการติดฉลากที่กำหนดโดยสหภาพยุโรปเพื่อช่วยให้คุณทราบว่าอาหารมีไขมันสูงและไขมันอิ่มตัวหรือไม่
ฉลากโภชนาการบนบรรจุภัณฑ์อาหารสามารถช่วยคุณลดไขมันทั้งหมดและไขมันอิ่มตัว (รวมถึงไขมันอิ่มตัวหรือไขมันอิ่มตัวด้วย)
ไขมันทั้งหมด Total fat
ไขมันอิ่มตัว Saturated fat
หากไขมันในอาหารของคุณมากเกินไป โดยเฉพาะไขมันอิ่มตัว ทำให้คอเลสเตอรอลในเลือดเพิ่มขึ้นได้ ซึ่งจะเพิ่มความเสี่ยงต่อการเป็นโรคหัวใจ
ปัจจุบันแนะนำให้ลดไขมันทั้งหมดและแทนที่ไขมันอิ่มตัวด้วยไขมันไม่อิ่มตัวบางส่วน
การลดไขมันอิ่มตัวเป็นเพียงแง่มุมหนึ่งในการลดความเสี่ยงของโรคหัวใจ โรคหลอดเลือดสมอง และโรคหัวใจและหลอดเลือดอื่นๆ ปัจจัยเสี่ยงอื่นๆ ได้แก่ การรับประทานเกลือและน้ำตาลมากเกินไป การมีน้ำหนักเกิน การสูบบุหรี่ และการขาดการออกกำลังกาย
เมื่อพูดถึงสุขภาพของหัวใจ คุณควรมุ่งเน้นไปที่อาหารโดยรวมของคุณมากกว่าสารอาหารแต่ละชนิด เช่น ไขมันหรือน้ำตาล การรับประทานอาหารที่สมดุล และมีคุณค่าทางโภชนาการถือเป็นหนึ่งในวิธีที่ดีที่สุดในการลดความเสี่ยงในการเกิดโรคหัวใจ และหลอดเลือด
การเลือกไขมัน
ไขมันไม่อิ่มตัวเชิงเดี่ยวและไขมันไม่อิ่มตัวเชิงซ้อนให้กรดไขมันที่จำเป็นและวิตามินที่ละลายในไขมัน ดังนั้นจึงเป็นส่วนสำคัญของอาหารของคุณ
หากเป็นไปได้ให้แทนที่ไขมันอิ่มตัวด้วยไขมันไม่อิ่มตัวเชิงเดี่ยวและไม่อิ่มตัวเชิงซ้อนในปริมาณเล็กน้อย
ปกติคนไม่ควรจะรับอาหารไขมันอิ่มตัวไม่เกินวันละ30 กรัม ในผู้ชาย 20 กรัมในผู้หญิง
ชนิดไขมัน |
พบในอาหาร |
ไขมันไม่อิ่มตัวเชิงเดี่ยว Monounsaturated รับประทานไม่เกินตามเกณฑ์ ไขมันนี้จะลดคอเลสเตอรอลในเลือด |
อะโวคาโด มะกอก น้ำมันมะกอก น้ำมันคาโนล่า ถั่วลิสง |
ไขมันไม่อิ่มตัวเชิงซ้อน Polyunsaturated รับประทานไม่เกินตามเกณฑ์ ไขมันนี้จะลดคอเลสเตอรอลในเลือด |
ปลา น้ำมันถั่วเหลือง น้ำมันงา น้ำมันข้าวโพด เมล็ดงา เมล็ดทานตะวัน วอลนัท |
ไขมันอิ่มตัว Saturated ให้เปลี่ยนไขมันอิ่มตัวเป็นไขมันไม่อิ่มตัว ไขมันอิ่มตัวทำให้คอเลสเตอรอลในเลือดสูง |
พบมากในเนื้อที่ผ่านขบวนการผลิตเช่น ไส้กรอก แฮม เบอร์เกอร์ เนื้อติดมัน เนยแข็ง นมครบส่วน น้ำมันหมู น้ำมันปาล์ม น้ำมันมะพร้าว |
ไขมันทรานส์ Trans รับประทานให้น้อยที่สุด ไม่เกินร้อยละ1ของพลังงานทั้งหมด ไขมันนี้จะทำให้คอเลสเตอรอลในเลือดเพิ่ม |
อาหารทอด เค้ก คุกกี้ เนยเทียม อาหารขยะ |
คำแนะนำสำหรับการบริโภคไขมัน
เนื่องจากไขมันในอาหารบางชนิดอาจมีประโยชน์และบางชนิดอาจเป็นอันตรายต่อสุขภาพของคุณ การรู้ว่าคุณกำลังรับประทานไขมันชนิดใดและเป็นไปตามคำแนะนำระดับชาติหรือไม่ แนวทางการบริโภคอาหารสำหรับชาวอเมริกันเสนอคำแนะนำเกี่ยวกับการบริโภคไขมันในอาหาร
ต่อไปนี้เป็นคำแนะนำและแหล่งที่มาทั่วไปของไขมันในอาหารแต่ละประเภท โปรดทราบว่าอาหารหลายชนิดมีไขมันต่างกันและแต่ละประเภทมีระดับต่างกัน ตัวอย่างเช่น เนยมีไขมันไม่อิ่มตัว แต่ส่วนใหญ่ของไขมันทั้งหมดเป็นไขมันอิ่มตัว และน้ำมันคาโนลามีเปอร์เซ็นต์ไขมันไม่อิ่มตัวเชิงเดี่ยวสูง แต่ก็มีไขมันไม่อิ่มตัวเชิงซ้อนและไขมันอิ่มตัวในปริมาณที่น้อยกว่าด้วย
แนวทางการบริโภคอาหารสำหรับชาวอเมริกัน ปี 2010
ตามคำแนะนำให้รับประทานไขมันอิ่มตัวได้ร้อยละ 7 ของพลังงานทั้งหมด โดยทั่วไปคนเรารับประทานอาหารเฉลี่ย 2000 แคลอรี เพราะฉนั้นจะรับประทานไขมันอิ่มตัวได้ 2000คูณ0.07 เท่ากับ 140 แคลอรี ไขมัน 1 กรัมได้พลังงาน 9 แคลอรี นำ140 แคลอรี่ หารด้วย 9 เพื่อให้ได้ไขมันอิ่มตัวประมาณวันละ 15 กรัม ให้ตรวจสอบจากฉลากอาหารว่ามีไขมันอิ่มตัวเท่าไร และรับประทานอาหารโดยจำกัดไขมันอิ่มตัวมิให้เกิน
คำแนะนำเรื่องการรับประทานไขมัน
| ชนิดของไขมัน | คำแนะนำ |
| ปริมาณไขมันรวม | แนะนำให้รับประทานไขมันร้อยละ25-35ของพลังงาน สำหรับคนปกติที่รับประทานอาหารวันละ 2000แคลอรีจะรับประทานไขมันได้วันละ 44- 78 กรัม |
| ไขมันไม่อิ่มตัวเชิงเดี่ยว | ยังไม่มีข้อกำหนดปริมาณจำกัด ให้รับประทานปริมาณภายใตข้อจำกัดของพลังงานที่ได้รับจากไขมัน |
| ไขมันเชิงซ้อน | ยังไม่มีข้อกำหนดปริมาณจำกัด ให้รับประทานปริมาณภายใตข้อจำกัดของพลังงานที่ได้รับจากไขมัน |
| Omega-3 | ยังไม่มีข้อกำหนดปริมาณจำกัด ให้รับประทานปริมาณภายใตข้อจำกัดของพลังงานที่ได้รับจากไขมัน |
| ไขมันอิ่มตัว | จำกัดรับได้ไม่เกินร้อยละ10ของพลังงานทั้งหมด สำหรับผู้ที่เสี่ยงต่อการเกิดโรคหัวใจให้รับได้ไม่เกินร้อยละ7ของพลังงานทั้งหมด คนทั่วไปรับ 2000แคลอรีจะรับไขมันอิ่มตัวได้ 22 กรัม( 10%) 15กรัม(7%) |
| ไขมันทรานส์ | จำกัดไม่เกินร้อยละ1 ของพลังงานทั้งหมดหรือปริมาณ 2.2 กรัม |
| คอเลสเตอรอล | รับประทานน้อยกว่า 300 กรัม สำหรับผู้ที่เสี่ยงต่อโรคหัวใจรับได้ไม่เกินวันละ200กรัม |
วิธีลดไขมันในเลือด
การเปลี่ยนแปลงวิถีชีวิต
หากคุณต้องการลดระดับคอเลสเตอรอล สิ่งที่ดีที่สุดอย่างหนึ่งที่คุณสามารถทำได้คือการเปลี่ยนแปลงวิถีชีวิต เช่น การรับประทานอาหารและการออกกำลังกาย ด้านล่างนี้คือพฤติกรรมการใช้ชีวิตที่คุณสามารถเปลี่ยนแปลงได้ เพื่อช่วยให้ระดับคอเลสเตอรอลอยู่ในช่วงปกติ:
รับประทานอาหารที่มีประโยชน์ต่อหัวใจ แผนการรับประทานอาหารที่ดีต่อหัวใจมักจะจำกัดปริมาณของไขมันอิ่มตัว(รับปประทานไม่เกินร้อยละ10ของพลังที่ได้รับแต่ละวัน) และไขมันทรานส์ที่คุณรับประทาน ในขณะที่รับประทานไขมันไม่อิ่มตัวที่ดีต่อสุขภาพมากขึ้น พร้อมกับผลไม้ ผัก เมล็ดธัญพืช และโปรตีนไม่ติดมัน 6 ตัวอย่างของรูปแบบการรับประทานอาหารที่มีประโยชน์ต่อหัวใจ ได้แก่
รักษาน้ำหนักให้แข็งแรง
ระดับคอเลสเตอรอลสูงสามารถส่งผลกระทบต่อทุกคน โดยไม่คำนึงถึงน้ำหนัก อย่างไรก็ตามการมีน้ำหนักตัวมากเกินไปก็เป็นปัจจัยเสี่ยงของระดับคอเลสเตอรอลที่ผิดปกติได้ หากคุณมีน้ำหนักเกิน การลดน้ำหนักแม้เพียงเล็กน้อยก็สามารถช่วยให้ระดับคอเลสเตอรอลของคุณดีขึ้นได้
ให้ออกกำลังกาย
แนะนำให้ผู้ใหญ่ออกกำลังระดับปานกลางอย่างน้อย 150 นาทีต่อสัปดาห์ หรือประมาณ 30 นาทีต่อวันในสัปดาห์
จัดการระดับความเครียดของคุณ
การศึกษาพบว่าความเครียดเรื้อรังอาจลดคอเลสเตอรอล HDL และเพิ่มคอเลสเตอรอล LDL
เลิกสูบบุหรี่หากคุณสูบบุหรี่
การสูบบุหรี่สามารถเพิ่มคอเลสเตอรอล LDL และลดคอเลสเตอรอล HDL ได้ คอเลสเตอรอล HDL ถือว่า "ดี" เพราะช่วยขจัดคอเลสเตอรอลส่วนเกินออกจากเนื้อเยื่อของคุณ การมี HDL มากขึ้นสามารถช่วยลดความเสี่ยงต่อโรคหัวใจได้
รับประทานอาหารที่ไม่มีไขมันเลยดีไหม
เคล็ดลับในการเลือกอาหารที่มีไขมันในอาหารประเภทที่ดีที่สุด
ตอนนี้คุณรู้แล้วว่าไขมันในอาหารประเภทใดที่ดีต่อสุขภาพหรือไม่ดีต่อสุขภาพ และปริมาณที่ควรรวมเข้าไป คุณจะปรับอาหารของคุณอย่างไรให้เป็นไปตามแนวทางการบริโภคอาหาร
เคล็ดลับที่จะช่วยคุณเพิ่มไขมันในอาหารของคุณ
| Type of fat | Total fat (g) | Sat(g) | Mono (g) | Poly (g) | อุณหภูมิเกิดควัน |
|---|---|---|---|---|---|
| Sunflower oil | 100 | 11 | 20 | 69 | 225 °C (437 °F) |
| Sunflower oil (มีการตัดแต่งพันธุกรรม) | 100 | 12 | 84 | 4 | |
| Soybean oil | 100 | 16 | 23 | 58 | 257 °C (495 °F) |
| Canola oil | 100 | 7 | 63 | 28 | 205 °C (401 °F) |
| Olive oil | 100 | 14 | 73 | 11 | 190 °C (374 °F) |
| Corn oil | 100 | 15 | 30 | 55 | 230 °C (446 °F) |
| Peanut oil | 100 | 17 | 46 | 32 | 225 °C (437 °F) |
| Rice bran oil | 100 | 25 | 38 | 37 | 250 °C (482 °F) |
| Vegetable shortening | 71 | 23 | 8 | 37 | 165 °C (329 °F) |
| Lard | 100 | 39 | 45 | 11 | 190 °C (374 °F) |
| Suet | 94 | 52 | 32 | 3 | 200 °C (392 °F) |
| Butter | 81 | 51 | 21 | 3 | 150 °C (302 °F) |
| Coconut oil | 100 | 86 | 6 | 2 | 177 °C (351 °F) |
เมื่อใช้ความร้อนน้ำมันมะกอก และน้ำมันคาโนล่าจะเกิดสาร Aldehydes น้อยกว่าน้ำมันดอกทานตะวันและน้ำมันข้าวโพด 20 เท่า สาร Aldehydes นี้จะเป็นสารที่ทำให้เกิดมะเร็งไม่ว่าจะเกิดจากการสูดดมหรือการรับประทาน
การใช้น้ำมันอย่าปลอดภัย
สารพิษที่เกิดจากการใช้น้ำมัน
ไขมันไม่อิ่มตัวเชิงซ้อน(หลายตำแหน่ง)มีประโยชน์ในการลดไขมันในเลือดและป้องกันโรคหัวใจ แต่หากเราเก็ไขมันให้ถูกแสงทำให้เกิดสารพิษทีละน้อย แต่หากทำอาหารอุณหภูมิมากกว่าจุดเกิดควันก็จะเกิดสารซึ่งทำให้เกิดโรคมะเร็งและหลอดเลือดหัวใจ ส่วนไขมันอิ่มตัวจะทนความร้อนได้ดี แต่เนื่องจากเป็นไขมันิ่มตัวหากรับประทานมากจะทำให้เกิดโรคหัวใจและหลอดเลือด แต่เกิดสารพิษน้อยเมื่อเจอความร้อนสูง
ส่วนไขมันไม่อิ่มตัวเชิงเดี่ยว(หนึ่งตำ)แหน่งหากเป็น extra virgin หรือ virgin หากรับประทานสดจะมีคุณค่าทางอาหารสูง และคุณค่าทางอาหารจะลดลงเมื่อเจอความร้อน แต่เกิดสารพิษไม่มาก
สรุป
วิธีลดไตรกลีเซอไรด์ตามธรรมชาติ
เพื่อเพิ่มระดับคอเลสเตอรอล HDL ของคุณ
ไขมันเลว
ไขมันเลวคือไขมันที่รับประทานเข้าไปแล้วส่งผลเสียต่อสุขภาพ ที่สำคัญได้แก่
ไขมันดี
ไขมันดีมักจะทำมาจากเมล็ดพืช ถั่ว มีด้วยกันสองชนิดคือ ไขมันไม่อิ่มตัวเชิงเดี่ยว monounsaturated fats และไขมันไม่อิ่มตัวเชิงซ้อน polyunsaturated fats
ส่วนไขมัน Omega-6 fatty acids จะป้องกันโรคหัวใจ อาหารที่มีไขมันชนิดนี้คือน้ำมันพืช เช่น น้ำมัดอกทานตะวัน น้ำมันถั่วเหลือง น้ำมันข้าวโพด
ทบทวนวันที่ 1/2/2566
โดย นายแพทย์ ประพันธ์ ปลื้มภาณุภัทร อายุรแพทย์,แพทย์เวชศาสตร์ครอบครัว