Overview
Orthostatic hypotension — also called postural hypotension — is a form of low blood pressure that happens when you stand up from sitting or lying down. Orthostatic hypotension can make you feel dizzy or lightheaded, and maybe even faint.
Orthostatic hypotension may be mild and last for less than a few minutes. However, long-lasting orthostatic hypotension can signal more-serious problems, so it's important to see a doctor if you frequently feel lightheaded when standing up.
Occasional (acute) orthostatic hypotension is usually caused by something obvious, such as dehydration or lengthy bed rest, and is easily treated. Chronic orthostatic hypotension is usually a sign of another health problem, so treatment varies.
Symptoms
The most common symptom is lightheadedness or dizziness when you stand up after sitting or lying down. Symptoms usually last less than a few minutes.
Orthostatic hypotension signs and symptoms include:
- Feeling lightheaded or dizzy after standing up
- Blurry vision
- Weakness
- Fainting (syncope)
- Confusion
- Nausea
When to see a doctor
Occasional dizziness or lightheadedness may be fairly minor — triggered by mild dehydration, low blood sugar or overheating. Dizziness or lightheadedness may also happen when you stand after sitting for a long time. If these symptoms happen only occasionally, there's likely no cause for concern.
It's important to see your doctor if you experience frequent symptoms of orthostatic hypotension because they can signal serious problems. It's even more urgent to see a doctor if you lose consciousness, even for just a few seconds.
Keep a record of your symptoms, when they occurred, how long they lasted and what you were doing at the time. If these occur at dangerous times, such as while driving, discuss this with your doctor.
Causes
When you stand up, gravity causes blood to pool in your legs and abdomen. This decreases blood pressure because there's less blood circulating back to your heart.
Normally, special cells (baroreceptors) near your heart and neck arteries sense this lower blood pressure. The baroreceptors send signals to centers in your brain, which signals your heart to beat faster and pump more blood, which stabilizes blood pressure. These cells also narrow the blood vessels and increase blood pressure.
Orthostatic hypotension occurs when something interrupts the body's natural process of counteracting low blood pressure. Many different conditions can cause orthostatic hypotension, including:
- Dehydration. Fever, vomiting, not drinking enough fluids, severe diarrhea and strenuous exercise with excessive sweating can all lead to dehydration, which decreases blood volume. Mild dehydration can cause symptoms of orthostatic hypotension, such as weakness, dizziness and fatigue.
- Heart problems. Some heart conditions that can lead to low blood pressure include extremely low heart rate (bradycardia), heart valve problems, heart attack and heart failure. These conditions prevent your body from responding rapidly enough to pump more blood when standing up.
- Endocrine problems. Thyroid conditions, adrenal insufficiency (Addison's disease) and low blood sugar (hypoglycemia) can cause orthostatic hypotension, as can diabetes — which can damage the nerves that help send signals regulating blood pressure.
- Nervous system disorders. Some nervous system disorders, such as Parkinson's disease, multiple system atrophy, Lewy body dementia, pure autonomic failure and amyloidosis, can disrupt your body's normal blood pressure regulation system.
- After eating meals. Some people experience low blood pressure after eating meals (postprandial hypotension). This condition is more common in older adults.
Risk factors
The risk factors for orthostatic hypotension include:
- Age. Orthostatic hypotension is common in those who are age 65 and older. Special cells (baroreceptors) near your heart and neck arteries that regulate blood pressure can slow as you age. It also may be harder for an aging heart to beat faster and compensate for drops in blood pressure.
-
Medications. These include medications used to treat high blood pressure or heart disease, such as diuretics, alfa blockers, beta blockers, calcium channel blockers, angiotensin-converting enzyme (ACE) inhibitors and nitrates.
Other medications that may increase your risk of orthostatic hypotension include medications used to treat Parkinson's disease, certain antidepressants, certain antipsychotics, muscle relaxants, medications to treat erectile dysfunction and narcotics.
Using medications that treat high blood pressure in combination with other prescription and over-the-counter medications may cause low blood pressure.
- Certain diseases. Some heart conditions, such as heart valve problems, heart attack and heart failure; certain nervous system disorders, such as Parkinson's disease; and diseases that cause nerve damage (neuropathy), such as diabetes, increase the risk of low blood pressure.
- Heat exposure. Being in a hot environment can cause heavy sweating and possibly dehydration, which can lower your blood pressure and trigger orthostatic hypotension.
- Bed rest. If you have to stay in bed a long time because of an illness, you may become weak. When you try to stand up, you may experience orthostatic hypotension.
- Pregnancy. Because your circulatory system expands rapidly during pregnancy, blood pressure is likely to drop. This is normal, and blood pressure usually returns to your pre-pregnancy level after you've given birth.
- Alcohol. Drinking alcohol can increase your risk of orthostatic hypotension.
Complications
Persistent orthostatic hypotension can cause serious complications, especially in older adults. These include:
- Falls. Falling down as a result of fainting (syncope) is a common complication in people with orthostatic hypotension.
- Stroke. The swings in blood pressure when you stand and sit as a result of orthostatic hypotension can be a risk factor for stroke due to the reduced blood supply to the brain.
- Cardiovascular diseases. Orthostatic hypotension can be a risk factor for cardiovascular diseases and complications, such as chest pain, heart failure or heart rhythm problems.
Diagnosis
Your doctor's goal in evaluating orthostatic hypotension is to find the underlying cause, and determine appropriate treatment for any health problems that may cause your low blood pressure. The cause isn't always known.
Your doctor may review your medical history, review your symptoms and conduct a physical examination to help diagnose your condition.
Your doctor also may recommend one or more of the following:
- Blood pressure monitoring. Your doctor will measure your blood pressure both while you're sitting and while you're standing and will compare the measurements. Your doctor will diagnose orthostatic hypotension if you have a drop of 20 millimeters of mercury (mm Hg) in your systolic blood pressure or a drop of 10 mm Hg in your diastolic blood pressure within two to five minutes of standing up, or if standing causes signs and symptoms.
- Blood tests. These can provide information about your overall health, including low blood sugar (hypoglycemia) or low red blood cell levels (anemia), both of which can cause low blood pressure.
-
Electrocardiogram (ECG or EKG). This noninvasive test detects irregularities in your heart rhythm or heart structure, and problems with the supply of blood and oxygen to your heart muscle.
During this painless, noninvasive test, soft, sticky patches (electrodes) are attached to the skin of your chest, arms and legs. The patches detect your heart's electrical signals while a machine records them on graph paper or displays them on a screen.
Sometimes, heart rhythm abnormalities come and go, and an ECG won't find any problems. If this happens, you may be asked to wear a 24-hour Holter monitor to record your heart's electrical activity as you go about your daily routine.
-
Echocardiogram. In this noninvasive exam, sound waves are used to produce a video image of your heart. Sound waves are directed at your heart from a wandlike device (transducer) that's held on your chest.
The sound waves that bounce off your heart are reflected through your chest wall and processed electronically to provide video images of your heart in motion to detect underlying structural heart disease.
- Stress test. A stress test is performed while you're exercising, such as walking on a treadmill. Or you may be given medication to make your heart work harder if you're unable to exercise. When your heart is working harder, your heart will be monitored with electrocardiography, echocardiography or other tests.
- Tilt table test. A tilt table test evaluates how your body reacts to changes in position. You'll lie on a flat table that tilts to raise the upper part of your body, which simulates the movement from a horizontal to standing position. Your blood pressure is taken frequently as the table is tilted.
- Valsalva maneuver. This noninvasive test checks the functioning of your autonomic nervous system by analyzing your heart rate and blood pressure after several cycles of a type of deep breathing: You breathe in deeply and push the air out through your lips, as if you were trying to blow up a stiff balloon.
Treatment
The goal of treatment for orthostatic hypotension is to restore normal blood pressure. That usually involves increasing blood volume, reducing the pooling of blood in your lower legs and helping blood vessels to push blood throughout your body.
Treatment often addresses the underlying cause — dehydration or heart failure, for example — rather than the low blood pressure itself.
For mild orthostatic hypotension, one of the simplest treatments is to sit or lie down immediately after feeling lightheaded upon standing. Your symptoms should disappear.
When low blood pressure is caused by medications, treatment usually involves changing the dose of the medication or stopping it entirely.
Orthostatic hypotension treatments include:
-
Lifestyle changes. Your doctor may suggest several lifestyle changes, including drinking enough water; drinking little to no alcohol; avoiding overheating; elevating the head of your bed; avoiding crossing your legs when sitting; and standing up slowly.
If you don't also have high blood pressure, your doctor might suggest increasing the amount of salt in your diet. If your blood pressure drops after eating, your doctor may recommend small, low-carbohydrate meals.
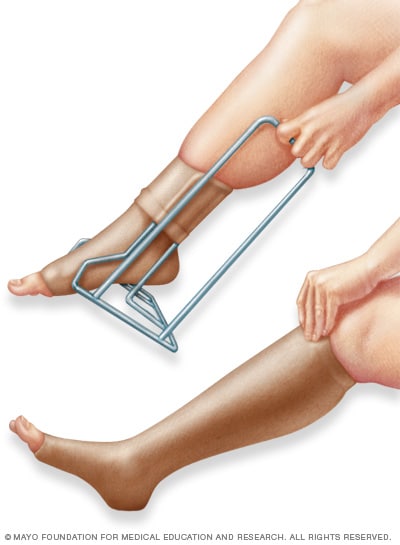
- Compression stockings. Compression stockings and garments or abdominal binders may help reduce the pooling of blood in your legs and reduce the symptoms of orthostatic hypotension.
-
Medications. Several medications, either used alone or together, can be used to treat orthostatic hypotension. For example, the drug fludrocortisone is often used to help increase the amount of fluid in your blood, which raises blood pressure. Midodrine raises standing blood pressure levels by limiting expansion of your blood vessels, which in turn raises blood pressure.
Droxidopa (Northera) may be prescribed to treat orthostatic hypotension associated with Parkinson's disease, multiple system atrophy or pure autonomic failure.
Other medications, such as pyridostigmine (Regonol, Mestinon), nonsteroidal anti-inflammatory drugs (NSAIDs), caffeine and epoetin (Epogen, Procrit, others), are sometimes used, too, either alone or with other medications for people who aren't helped with lifestyle changes or other medications.