มะเร็งไฝ Melanoma
เป็นมะเร็งผิวหนังชนิดหนึ่งที่แพร่กระจายเร็วมาก เกิดจากเซลล์สร้างสีผิว melanocyte การที่จะเข้าใจโรคนี้ท่านจะต้องเข้าใจโครงสร้างของผิวหนัง
โครงสร้างของผิวหนัง
- ผิวหนังเป็นอวัยวะที่ห่อหุ้มร่างกายทำหน้าที่ป้องกัน ความร้อน แสง การติดเชื้อ ควบคุมอุณหภูมิของร่างกาย และสร้างวิตามินดีผิวหนังประกอบด้วยเซลล์สองชั้น
- ชั้น epidermis เป็นชั้นนอกสุดประกอบด้วยชั้นบนสุดเป็น squamous เซลล์รองลงมาได้แก่ basal cell โดยมี melanocyte อยู่ใต้ subcutaneous
- ชั้น dermis เป็นชั้นที่อยู่ของต่อมขน ต่อมเหงื่อ ต่อมไขมัน หลอดเลือด
melanocyte เป็นตัวสร้างสีผิว melanin เมื่อผิวถูกแสงทำให้สีผิวเข็มขึ้น ไฝเป็นกลุ่มของ melanocyte ที่อยู่รวมกันมักเกิดในช่วงอายุ 10-40 ปี อาจจะแบน หรือนูน สีอาจเป็นสีชมพู หรือสีน้ำตาล รูปร่างกลม หรือวงรีไฝมักจะไม่เปลี่ยนแปลงขนาดหรือสีตัดออกแล้วไม่กลับเป็นซ้ำ
Melamoma
เป็นมะเร็งที่เกิดจากเซลล์ melanocyte ที่แบ่งตัวนอกเหนือการควบคุมของร่างกาย ถ้าเกิดที่ผิวหนังเรียก cutaneous melanoma เกิดที่ตาเรียก ocular melanoma โดยทั่วไปเกิดบริเวณลำตัว ขา ถ้าคนผิวดำมักเกิดที่เล็บ โดยทั่วไปมะเร็งแพร่กระจายไปยังต่อมน้ำเหลืองและอาจพบที่อวัยวะอื่นๆได้เรียก metastasis melanoma
ปัจจัยเสี่ยงของการเกิดมะเร็ง
- ประวัติครอบครัวเป็นมะเร็งไฝ จะมีความเสี่ยงเพิ่มมากกว่า 2 เท่าดังนั้นสมาชิกในครอบครัวควรได้รับการตรวจจากแพทย์
- Dysplastic nevi ไฝที่มีลักษณะชิ้นเนื้อแบบนี้จะมีโอกาสเป็นมะเร็งสูง
- เคยเป็น melanoma
- ภูมิคุ้มกันอ่อนแอ เช่น AIDS
- ผู้ที่มีโรคประจำตัวต้องใช้บางชนิดซึ่งจะทำให้เกิดการแพ้แสงแดดง่ายขึ้น
- มีไฝจำนวนมาก เช่นมากกว่า 50 เม็ดจะมีโอกาสเป็นมะเร็งมาก
- แสง ultraviolet ควรสวมเสื้อแขนยาวและหมวกเพื่อกันแสง ควรหลีกเลี่ยงแสงแดดเวลา10-16.00 น.ควรทาครีมกันแสงร่วมด้วย
- เคยถูกแสงจนไหม้เมื่อวัยเด็ก ดังนั้นควรป้องกันไม่ให้เด็กสัมผัสแสงแดด
- สีผิว ผิวขาวมีโอกาสเกิดมะเร็งได้ง่ายกว่าผิวคล้ำ
ปัจจัยเสี่ยงของการเกิดมะเร็งผิวหนัง
จากการศึกษาพบสาเหตุสำคัญของการเกิดมะเร็งผิวหนังที่พบบ่อยได้แก่
- แสงแดด แสงแดดจะมีรังสี UV ซึ่งจะทำลายผิวหนังและเพิ่มความเสี่ยงในการเกิดมะเร็งผิวหนัง
- ผิวพุพองเนื่องจากแดดเผา หากท่านเคยเป็นครั้งหนึ่งในชีวิต ท่านจะเสี่ยงต่อการเกิดมะเร็งผิวหนัง ผู้ที่ผิวไหม้จากแดดง่ายจะเสี่ยงต่อมะเร็งผิวหนัง
- ผู้ที่ต้องสัมพัสแสงแดด หากท่านมีอาชีพ หรือท่านต้องได้รับแสงแดดตลอดเวลาท่านจะเสี่ยงต่อการเกิดมะเร็งผิวหนัง
- การอาบรังสีเพื่อทำผิวสีแทน ท่านจะเสี่ยงต่อการเกิดมะเร็งผิวหนัง
แสงแดดสามารถสะท้อนจากทราย น้ำ หิมะ หรออาคาร ทะลุเสื้อผ้าบางๆ
อาการของมะเร็งไฝ
อาการเริ่มแรกมักเริ่มเกิดการเปลี่ยนแปลง ขนาด สี รูปร่าง ขอบ บางรายอาจมีอาการคัน มีขุยหากเป็นมากขึ้นอาจมีการเปลี่ยนแปลงของความแข็ง หากพบมะเร็งเริ่มต้นการรักษาจะหายขาด แต่หากรุกลามเข้าใต้ผิวหนังมะเร็งอาจแพร่กระจายไปยังอวัยวะอื่น
Asymmetry รูปร่างไม่สมดุล |
Border ขอบไม่เรียบ เป็นรอยขรุขระ |
 |
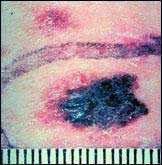 |
Color มีการเปลี่ยนของสี |
Diameter ขนาดใหญ่ขึ้น |
 |
 |
การวินิจฉัย
หากแพทย์สงสัยว่าไฝที่เห็นว่าจะเป็นมะเร็งแพทย์จะตัดก้อนนั้นส่งพยาธิแพทย์ตรวจด้วยกล้องจุลทัศน์ หากก้อนนั้นใหญ่มากแพทย์จะตัดเพียงบางส่วนส่งตรวจ ถ้าพบเซลล์มะเร็งแพทย์จะตรวจพิเศษเพิ่มเพื่อตรวจดูว่ามะเร็งแพร่กระจายไปยังอวัยวะอื่นหรือยัง
การรักษา
หลังจากวินิจฉัยและทราบการแพร่กระจายของโรคแพทย์จะวางแผนการรักษา ก่อนการรักษาควรจดบันทึกคำถามเพื่อถามแพทย์ดังตัวอย่าง
- การวินิจฉัยของแพทย์
- มะเร็งแพร่กระจายไปหรือยัง
- ควรจะรักษาด้วยวิธีใดดีที่สุด และแพทย์เลือกวิธีใด
- โอกาสที่จะประสบผลสำเร็จมีมากหรือไม่
- เราจะทราบอย่างไรว่าการรักษาได้ผล
- การรักษาจะสิ้นสุดเมื่อใด
- จะดูแลตัวเองระหว่างการรักษาอย่างไร
- ผลข้างเคียงของการรักษามีอะไรบ้าง
- จะเจ็บปวดหรือไม่ และจะใช้ยาอะไรในการควบคุม
- หลังการผ่าตัดต้องรักษาอย่างอื่นหรือไม่
วิธีการรักษา
- การผ่าตัด เป็นการรักษามาตรฐานแพทย์จะพยายามตัดเนื้อร้ายออกให้หมดร่วมทั้งต่อมน้ำเหลืองที่ใกล้เนื้อร้าย ถ้ามะเร็งแพร่กระจายไปอวัยวะอื่นแพทย์จะให้การรักษาอย่างอื่น
- เคมีบำบัด เป็นการให้สารเคมีเพื่อฆ่าเซลล์มะเร็งโดยอาจเป็นยากินหรือยาฉีด
- รังสีรักษาเป็นการฆ่ามะเร็งเฉพาะที่โดยเฉพาะมะเร็งที่แพร่กระจายไปยังอวัยวะอื่น เช่น สมอง ปอด ตับ
- การสร้างภูมิคุ้มกัน อาจให้ภูมิโดยการฉีด เช่นการให้ interferon หรือ interleukin โดยการกระตุ้นให้ร่างกายสร้างภูมิขึ้นมาเช่นการฉีดวัคซีน
ผลข้างเคียงของการรักษา
- การผ่าตัด อาจทำให้เกิดแผลเป็นบางรายเกิด keloid การตัดต่อมน้ำเหลืองอาจทำให้ขาหรือแขนบวม
- เคมีบำบัด การให้เคมีบำบัดอาจให้เกิดโลหิตจาง ติดเชื้อง่าย หรือเลือดออกง่าย ผมร่วง
- รังสีรักษา ทำให้ผมบริเวณที่ฉายรังสีร่วง อาจมีอาการอ่อนเพลีย
- การสร้างภูมิคุ้มกัน อาจมีอาการปวดเมื่อตามตัวเบื่ออาหาร ท้องร่วง
การผ่าตัด
แพทย์จะผ่าตัดเอาเนื้อมะเร็ง รวมทั้งเนื้อดีบางส่วนเพื่อให้แน่ใจว่าไม่มีมะเร็งหลงเหลือ วิธีการผ่าขึ้นกับชนิดของมะเร็ง ขนาดของมะเร็ง และตำแหน่งของมะเร็ง
- การผ่าตัดเอามะเร็งออก (Excisional) แพทย์จะผ่าเอามะเร็งและเนื้อดีบางส่วนออก และนำชิ้นเนื้อไปส่องกล้องจุลทัศนดูขอบว่ามีมะเร็งอยู่อีกหรือไม่ ตัดจนขอบแผลไม่มีมะเร็ง
- Mohs surgery เป็นการเลาะเนื้อเยื่อทีละชั้น และนำไปส่องจนกระทั่งไม่พบเซลล์มะเร็ง
- การจี้ไฟฟ้า(Electrodesiccation ) และการขูดแผล(curettage) วิธีการจะใช้อุปกรณ์คล้ายกับช้อนขูดบริเวณที่เป็นโรค และใช้เครื่องจี้เพื่อให้เลือดหยุดและฆ่าเซลล์มะเร็ง อาจจะต้องทำ 3-4 ครั้งจึงจะทำลายมะเร็งได้หมด
- การใช้ความเย็น (Cryosurgery) วิธีการนี้จะใช้กับมะเร็งแรกเริ่ม และผู้ป่วยไม่เหมาะสำหรับการผ่าตัด โดยการใช้ไนโตรเจนเหลวทายังบริเวณที่เป็นโรค ความเย็นจะทำลายเซลล์มะเร็งขณะเดียวกันก็จะทำลายเนื้อดี ทำให้เกิดการชา

สำหรับมะเร็งที่มีการแพร่กระจายไปต่อมน้ำเหลืองจะต้องมีการเลาะต่อมน้ำเหลืองออกบางส่วน
- เคมีบำบัด การใช้ยารักษามะเร็งอาจจะใช้ทาที่บริเวณเกิดโรคเช่นยา Fluorouracil ,Imiquimod หรืออาจจะใช้ยาฉีด
- การรักษาด้วยวิธี Photodynamic Therapy วิธีการทำ ฉีดสารเข้ากระแสเลือดเซลล์มะเร็งจะจับสารนั้น หลังจากนั้นก็จะให้แสงคลื่นพิเศษซึ่งจะทำลายมะเร็งที่มีสารเคมีนั้น ส่วนเซลล์ปกติไม่ถูกทำลาย
- การใช้ Biological Therapy ดดยการฉีด interferon , interleukin-2. ซึ่งทำให้ภูมิแข็งแรงและฆ่าเซลล์มะเร็ง
- การใช้รังสีรักษา Radiation Therapy เป็นการฉายรังสีไปยังส่วนที่เป็นมะเร็ง